Lumbar Spinal Stenosis (LSS)
- Dr. Brian Abelson DC.
- Apr 28, 2023
- 16 min read
Updated: Mar 13, 2024

What is Lumbar Spinal Stenosis?
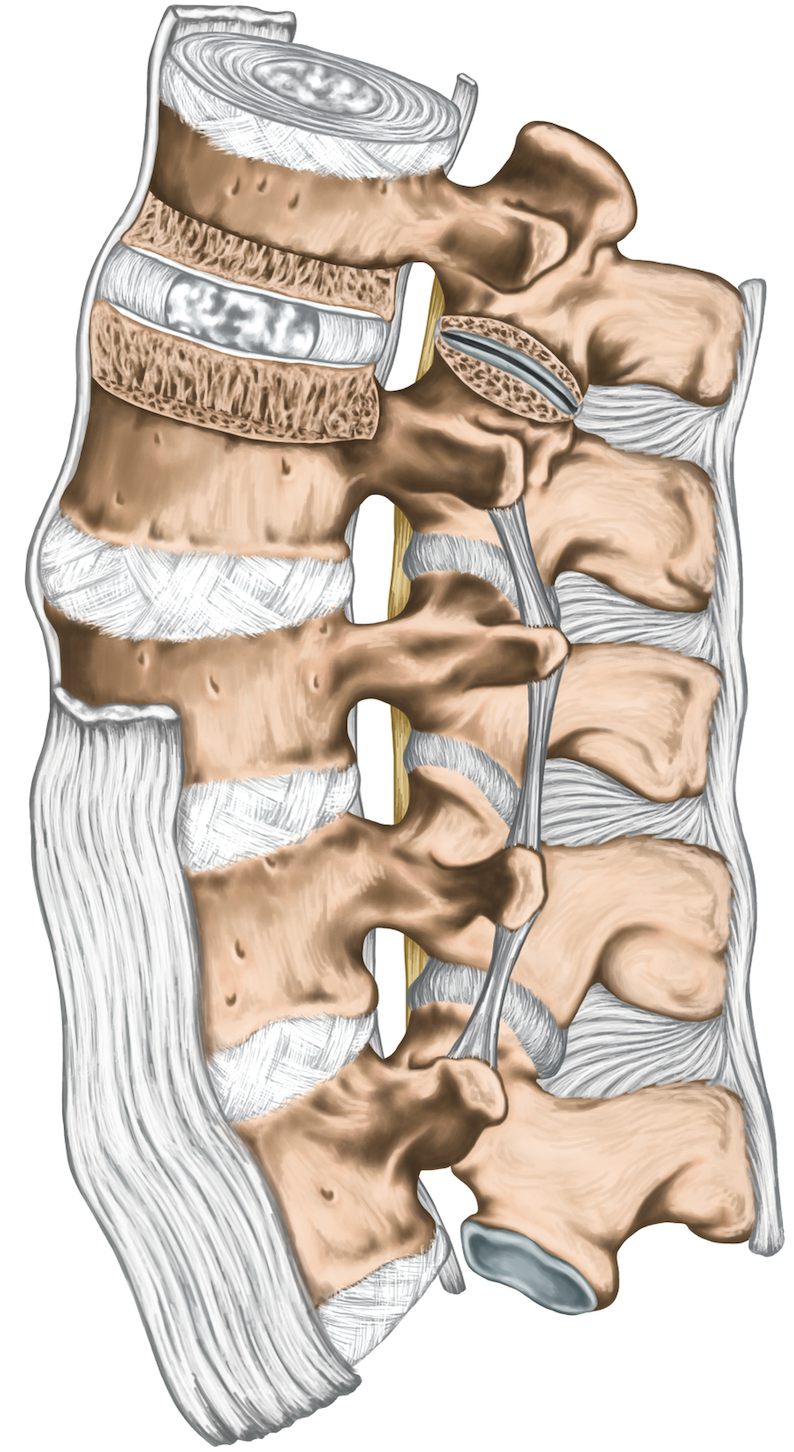
Lumbar Spinal Stenosis is one of the most common reasons for spinal surgery in patients over 65. Lumbar Spinal Stenosis is caused by a gradual narrowing of the central spinal canal, the lateral recess, or IVF (intervertebral foramen – a passage between the spinal canal and the periphery) in compression of the neurovascular structures of the spine. (1)
Lumbar Spinal Stenosis significantly impacts our healthcare system as it is a leading cause of disability in an aging population. Lumbar Spinal Stenosis causes more functional limitations than congestive heart failure, COPD (Chronic obstructive pulmonary disease), or Lupus. (2,9)
The good news is that Lumbar Spinal Stenosis often responds to a combination of exercise and manual therapy. Surgery is necessary for some patients but not for many others. In addition, spinal stenosis is a slow-progressing condition. This means that in most situations, you have time to improve your health and deal with this condition.

Symptoms of Lumbar Spinal Stenosis (LLS)
The symptoms of Lumbar Spinal Stenosis can vary depending on the severity of the condition and may include: (3,9)
Pain or discomfort in the lower back, buttocks, or legs.
Weakness or cramping in the legs (unilateral or bilateral). This is most often caused by neurogenic claudication. (Neurogenic means arising in the nervous system. Claudication refers to leg pain, heaviness, or weakness when walking).
Difficulty standing up straight or difficulty with prolonged standing.
Back pain decreases when bending forward (ordinary back pain often feels worse when bending forward in a flexed position). Clinicians refer to this symptom as a shopping cart sign.
Decreased balance.
Back pain is reduced by sitting (ordinary back pain usually increases with sitting).
Back pain or leg pain that increases with standing (ordinary back pain often feels better on standing).
Increased strength in the legs with sitting or lying down (regular back pain does not cause an increase or decrease in leg strength in the legs with a change of position).
Red Flag: Loss of bladder or bowel control; this is a red flag. See your medical practitioner immediately.
Causes of Lumbar Spinal Stenosis (LSS)
Osteoarthritis, damage to spinal discs, thickening of ligaments and inflammation are key causative factors in Lumbar Spinal Stenosis. (4)

Osteoarthritis
Spondylosis is the term used to describe osteoarthritis of the spine. Arthritis in the spine can cause intervertebral disc and facet joint degeneration, as well as the development of bone spurs, also known as osteophytes. As arthritis worsens, the spinal canal gradually narrows, which can result in the compression of both the spinal cord and nerve roots that exit from the foramina of the spine. This, in turn, leads to a loss of function and pain.
Tip: The good news is that by strengthening the muscles that stabilize the spine, you can dramatically decrease the process of osteoarthritis (osteophyte and bone spur formation) , and help to avoid the progression of LSS.

Spinal Disc Damage
Spinal discs can lose height, become stiff, and lose flexibility due to Degenerative Disc Disease (DDD), injury, and aging. In our twenties, the centre of spinal discs is jelly-like. It contains a high amount of fluid, enabling them to function as effective shock absorbers, distributing spinal forces and preventing harm. Regrettably, by the time most individuals reach the age of sixty, these same discs have become as rigid as a well-done steak, making them a source of neurovascular compression.
Tip: Lack of disc hydration is a major issue. Fortunately, exercise is a great way to increase hydration of spinal discs. When we exercise, we increase the blood supply to our spinal discs, thereby increasing hydration. This hydration increases disc height and promotes better shock absorption capacity.
Ligament Thickening
Ligaments in good condition have elasticity, meaning they can stretch when subjected to pressure and regain their original shape when the force is released. However, when ligaments are unhealthy, they tend to bunch up and lose their ability to recover their original shape. This can significantly contribute to Lumbar Spinal Stenosis.
Tip: The health of the spinal ligaments is closely linked to several factors, including the patient's present physical condition, level of physical activity, dietary habits, and smoking status. It's worth noting that Lumbar Spinal Stenosis patients should avoid smoking, as it is considered one of the most harmful activities for them.

Inflammation
Swelling, caused by inflammation, is a significant contributor to Lumbar Spinal Stenosis. Swelling restricts the smooth movement of neurological structures and alters the texture of ligaments, muscles, and fascia. Inflammation thickens ligaments, making them stiffer and less elastic, which raises the risk of developing Lumbar Spinal Stenosis.
Congenital Factors
Some people are born with a narrower spinal canal, which can increase the risk of developing spinal stenosis later in life.
Diagnosing Lumbar Spinal Stenosis
Diagnosing Lumbar Spinal Stenosis typically involves a combination of a physical examination, medical history, and imaging tests. During the physical exam, your healthcare provider will likely ask about your symptoms and perform a neurological exam to assess your leg reflexes, strength, and sensation.
Your healthcare provider may also order imaging tests such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans to get a detailed look at the structures of your spine and confirm the diagnosis of Lumbar Spinal Stenosis.
In some cases, your healthcare provider may also order a nerve conduction study or electromyography (EMG) to evaluate the function of your nerves and muscles.

Key Diagnosis Questions:
The International Delphi study stated 7 historical diagnostic questions that can be used to help identify Lumbar Spinal Stenosis. (5,9)
Does the patient experience leg or buttock pain when walking?
Does the patient flex forward to relieve symptoms?
Does the patient experience decreased pain when using a shopping cart or bicycle?
Does the patient have motor or sensory disturbances while walking?
Are the ‘pulses’ in the foot present and symmetric?
Does the patient have lower extremity weakness?
Does the patient have low back pain?

Differential Diagnosis of Lumbar Spinal Stenosis
When diagnosing a patient with Lumbar Spinal Stenosis, we also must consider other conditions that may mimic Lumbar Spinal Stenosis. For example, Osteoarthritis, Herniated Disc, Trochanteric Bursitis, Peripheral Neuropathy, or Vascular Claudication. (6,9)
Hip Osteoarthritis (OA)
There is a considerable cross-over in symptoms between Lumbar Spinal Stenosis and Hip OA. Hip OA also presents with gluteal, groin, lateral hip and leg pain when weight bearing.
Osteoarthritis can cause cartilage breakdown in the spine's joints, leading to bone spurs and narrowing of the spinal canal. You must consider that both conditions could occur simultaneously.
Herniated Disc
A herniated disc occurs when the soft inner material of a spinal disc pushes through the outer layer and presses on a nerve. This can cause pain and numbness in the back and legs.
Trochanteric Bursitis
With trochanteric bursitis, the patient often experiences lateral leg pain, which is increased by lying on the affected side. This is not the case with Lumbar Spinal Stenosis and is one way to differentiate between the conditions.
Peripheral Neuropathy
This condition involves damage to the peripheral nerves, which can cause pain, numbness, and weakness in the legs and feet.
Vascular Claudication
Vascular claudication is a leg pain that occurs due to decreased blood flow. Similar to Lumbar Spinal Stenosis, vascular claudication (caused by Peripheral Arterial Disease - PAD) causes increased pain with walking that is also relieved by rest. The difference is that the pain of vascular claudication is not relieved with forward flexion (shopping cart sign) or cycling as it is with Lumbar Spinal Stenosis. With Lumbar Spinal Stenosis, a change in position (forward flexion) will cause a decrease in symptoms; with PAD, all activity will have to be stopped to relieve symptoms.
Physical Examination
The following videos contain some common orthopedic and neurological examination procedures we use to diagnose spinal Lumbar Spinal Stenosis.
Low Back Examination - Effective Orthopaedic Testing - This video covers some common causes of low back pain and how to diagnose them using orthopedic examination procedures.

Hip Examination - Orthopaedic Testing This video goes through inspection and observation, palpation, Active and Passive Ranges of motion, and orthopedic examination of the Hip region.
Lower Limb Neuro Examination - The lower limb neurological examination is part of the overall neurological examination process. It assesses the motor and sensory neurons that supply the lower limbs.
Peripheral Vascular Examination - Key Points
A peripheral vascular examination is valuable for ruling out signs of vascular-related pathology. The detection and subsequent treatment of PVD can potentially mitigate cardiovascular and cerebrovascular complications. In this video, we review some common procedures we perform in daily clinical practice.

Treatment of Lumbar Spinal Stenosis
As previously mentioned, Lumbar Spinal Stenosis is a frequent cause of spinal surgery in patients over 65. However, just because surgery is prevalent, it doesn't imply that it should be the initial approach to addressing this condition or that surgery will inevitably be required.
Strong evidence suggests that manual therapy, coupled with exercise, should be the first course of action before considering surgery. Furthermore, even if surgery becomes necessary, traditional therapy (manual therapy + exercise) can significantly achieve better outcomes, both before and after surgery.
Some common manual therapy techniques used for Lumbar Spinal Stenosis include:
Spinal mobilization involves slow, rhythmic movements of the spine to improve joint mobility and decrease pain.
Soft tissue therapy involves applying pressure and manipulating soft tissues, such as muscles and ligaments, to decrease tension and improve blood flow.
Stretching: Your provider may guide you through specific stretches to improve flexibility and reduce symptoms.
Myofascial Release: This technique involves applying pressure to specific regions in the body to release tension and decrease pain.
Research shows that 33%-50% of patients (with mild to moderate symptoms) who receive conventional therapy show significant functional improvements. By improvement, I am referring to decreased levels of pain, overall improved function in activities of daily living, and an increased ability to walk. This change could be enough of an improvement to avoid surgery completely. (1, 7, 8,9)
It is interesting to note what research DOES NOT recommend. For example, the use of Tylenol, NSAIDs, opioids, neurogenic pain medications, muscle relaxants, and epidural steroidal injections are not recommended for the treatment of Lumbar Spinal Stenosis. Unfortunately, these are some of the most common forms of treatment prescribed for this condition. (9)
If a patient is in acute pain, is not sleeping, or cannot perform exercises due to pain, then pharmaceutical intervention makes sense. But only so they can sleep, perform their prescribed exercises, and receive manual therapy. (1, 7, 8,9)
Manipulation & Mobilization
Spinal Manipulation or Mobilization can be of great benefit in helping patients who suffer from Lumbar Spinal Stenosis. Think of the spine, from the neck to the lumbar region, as one functional unit that needs optimum mobility for load distribution. When your upper back and neck are mobile, flexible, and strong, then when you act, the force exerted is shared throughout the entire spine.
That is why we recommend that patients focus on both the symptomatic area (lumbar spine) and any other areas of spinal tension. The following videos provide examples of both manipulation and mobilization procedures. Both types of procedures are extremely effective, and we customize our recommendations and treatments based on the needs of each individual patient. (1) Click on the video for an example of lumbar spinal joint mobilization.

Joint Mobilization - Lumbar Spine
Many aspects need to be addressed when eliminating low back pain. One of the key aspects is joint mobility. Basically, our capacity to produce an unlimited variety of movements requires good joint integrity. No joint ever works in isolation. An injury in one joint often results in bio-mechanical compensations in adjacent and distant joints.
Soft Tissue Therapy
The following videos are examples of common MSR procedures we often use with our Stenosis patients. The quality of your soft tissues will directly affect the level of pain experienced and your ability to function.
Lumbar and Thoracic Spine Fascial Release - In many cases, the thoracolumbar fascia can be an important key to resolving chronic low back pain. The Thoracolumbar Fascia [TLF] is a large region of connective tissue.
Resolve Chronic Low Back Pain - One of the structures that must be addressed is the deep paraspinal muscles. The Deep Para-Spinals (transversospinalis) muscles often atrophy in chronic low back pain cases.

Exercise is Critical
Research shows that individuals who exercise regularly are less likely to suffer from spinal stenosis. When you are hurting, it may seem counterintuitive to exercise while you’re in pain, but it is not.
Think of exercise as a counter-inflammatory strategy. Exercise increases circulatory function, removes waste by-products, brings oxygen to the injury site, and reduces pain levels. It is a simple equation. The more inflammation, the more pain is experienced. Decrease the inflammation, and experience a corresponding decrease in pain.
In addition to reducing inflammation, exercise makes ligaments and fascia more pliable, less rigid, and less likely to compress neurological structures. Exercise also decreases swelling, thus reducing the amount of neurovascular compression. (1)

Aerobic Exercise
Walking, swimming, or cycling can help improve cardiovascular health and increase endurance without putting excessive stress on the spine.
Aerobic or cardiovascular exercise is about increasing aerobic capacity, circulatory function, and energy production. Aerobic exercise does this by increasing the density of capillaries in the muscles and increasing the level of mitochondrial function in the cells. When you have more capillaries, your cells can obtain more nutrients for repair and get rid of waste by-products more rapidly.
Aerobic exercise is all about increasing your capillary health. Aerobic exercise is essential when dealing with Lumbar Spinal Stenosis. It can make the difference between being symptom-free and being in constant pain. (10)
Your Aerobic Zone
When performing an aerobic exercise, you must work within your aerobic zone. This is the range within which you want your heart to operate while performing your aerobic exercise. Think of your aerobic zone as the base you must establish for rehabilitation.
Calculating your aerobic zone - Use the following formula to calculate your aerobic zone: (11)
Subtract your age from the number 220. For example, if I am 40 years old, then 220 - 40 = 180.
Obtain the low end of your aerobic range by multiplying the result of step 1 by 0.6. In our example: 180 * 0.6 = 108
Obtain the high end of your aerobic range by multiplying the result of step 1 by 0.7. In our example: 180 * 0.7 = 126
This is your aerobic heart rate zone. Work within this zone to develop your aerobic capacity. It is the zone which will best speed your recovery from an injury. If you work above this zone, you run the risk of injury. If you work below this zone, you will not achieve the maximum benefits of your aerobic warm-up.
We recommend our patients take a staggered approach to aerobic exercise.
In stage 1, we recommend 5 to 10 minutes of aerobic exercise for 3 to 5 days per week (riding a bike or swimming).
In stage 2, we recommend 15 to 20 minutes of aerobic exercise 4 to 7 days per week (riding a bike or swimming).
In stage 3, we recommend 30 to 60 minutes of aerobic exercise 5 to 7 days per week (riding a bike or swimming).
TIP: We highly recommend purchasing a heart monitor/watch to monitor aerobic activity. You will progress faster and be better able to monitor potential cardiovascular issues.

Walking
Lumbar spinal stenosis can make walking difficult and painful. For many, walking may not be the best type of exercise if you are suffering from lumbar spinal stenosis. In addition, it is very difficult to get into the aerobic zone with walking; biking and swimming are much better choices.
That does not mean you need to give up on walking! You need to keep walking. Think of walking as a ‘baseline test’, in which you slowly increase your distance as your pain-free walking capacity increases.
Walking is a low-impact activity that can help improve cardiovascular health, increase endurance, and reduce pain and other symptoms associated with Lumbar Spinal Stenosis in many cases.
Remember that if your legs are weak, you should NOT push yourself to walk further distances. Doing so could lead to further damage and weakness.
Daily Exercise Routine
The following video exemplifies some common exercises we prescribe to patients suffering from Lumbar Spinal Stenosis. You will notice that several of these exercises focus on hip mobility. Increasing hip mobility through exercise and manual therapy can often make the difference between pain-free or extreme pain with each step.

5 Best Exercises For Spinal Stenosis These are some common exercises we prescribe to patients suffering from Lumbar Spinal Stenosis.
General Recommendations
In addition to exercise and treatment, use the following pain avoidance strategies to deal with Lumbar Spinal Stenosis. These strategies are based on pain avoidance. With lumbar spinal stenosis, performing an activity that aggravates the condition may cause the patient to feel the effects of that action for several hours after.

Avoiding Pain-Causing Activities
Patients will often tell me how performing certain actions causes them pain. But, they keep performing those same actions repeatedly, exacerbating their condition and prolonging their pain. A good example is trying to stand up straight, even when it is one of the most painful positions for many people suffering from LSS.
Patients suffering from Lumbar Spinal Stenosis often show a bent-over, flexed posture. These patients tend to keep trying to straighten up when they are not ready and in constant pain. I keep telling my patients they should NOT force themselves to stand up straight. I tell them to straighten up only when their inflammation and swelling decrease. This is when the pressure on neurological structures is decreased, and they can move into an upright position without pain. Forcing yourself to stand up straight when suffering from LLS can increase pressure on the spinal cord, decreasing leg strength.
Extension Intolerance
Extension-intolerant Lumbar Spinal Stenosis is a type of Lumbar Spinal Stenosis where the patient experiences symptoms, such as pain and numbness when the lower back is extended. Extension-intolerant Lumbar Spinal Stenosis is more common in older adults and can be caused by degenerative changes in the spine. Patients with extension-intolerant Lumbar Spinal Stenosis may benefit from exercises and treatments focusing on flexion or forward bending of the spine rather than the extension.
The key to healing from LSS is to avoid any activity that forces you to bend backwards, as this position closes down the foramina and creates less space in the spinal channel. For example, reaching overhead for an item in a cupboard could cause pain for several hours.
Tip: You should only reintroduce new activities when you can start performing them without pain.

Use Braces, Canes and Walkers
Braces (elastic corset) can greatly benefit patients who suffer from Lumbar Spinal Stenosis, especially during a flareup. This is because the brace limits lateral flexion and the frequency of repetitive motion. This limits nerve root irritation a possible source of radicular pain. Braces can help the patient to remain active while reducing the chance of re-injury. In addition, the brace helps them sleep better by keeping the spine in a neutral position while sleeping.
Many patients avoid using walkers (or canes) out of fear of building a dependency, but they really should not. Just because they need it at certain times does not mean they will need it forever.
Using a walker (or can) when their symptoms are severe (during a flareup) or for a couple of days could greatly reduce the level of pain experienced. In addition, using the walker first thing in the morning or at the end of the day could help prevent a fall, and a possible hip or spinal fracture. When you feel better/stronger, you can get rid of the walker or cane.

Sleeping Positions
Finding the right sleeping position can be helpful for people with Lumbar Spinal Stenosis to reduce pain and improve the quality of sleep. Some recommended sleeping positions for people with Lumbar Spinal Stenosis include:
Side sleeping with a pillow between the knees: This can help to align the spine and reduce stress on the lower back.
Sleeping on the back with a pillow under the knees: This can help to reduce pressure on the lower back and promote proper spinal alignment.
Sleeping in a reclined position: This can help to reduce pressure on the lower back and may be helpful for people who experience symptoms when lying flat.
It is important to avoid sleeping on the stomach, as this can increase stress on the lower back and worsen symptoms of Lumbar Spinal Stenosis.

Conclusion
To summarize, Lumbar Spinal Stenosis is a prevalent issue affecting the elderly demographic, often leading to substantial functional constraints. The silver lining, however, is that this condition can frequently be mitigated through a combination of exercise and manual therapy, thus eliminating the need for surgery in many instances.
Several key factors, including osteoarthritis, spinal disc deterioration, ligament thickening, inflammation, and congenital aspects, contribute to Lumbar Spinal Stenosis. The diagnosis typically involves a physical examination, medical history review, and imaging tests.
Treatment strategies encompass manual techniques like spinal mobilization, soft tissue therapy, stretching, and myofascial release, alongside regular physical activity. Exercise reduces inflammation, enhances cardiovascular health, and boosts endurance.
Patients can achieve significant functional improvements by incorporating these treatment strategies, potentially bypassing surgical intervention. It's important to underline that pharmaceutical interventions such as Tylenol, NSAIDs, opioids, neurogenic pain medications, muscle relaxants, and epidural steroidal injections are NOT endorsed for treating Lumbar Spinal Stenosis.
Studies emphasize the critical role of exercise for individuals aiming to prevent or alleviate Lumbar Spinal Stenosis symptoms. Aerobic exercise is particularly beneficial as it can decide between pain-free and enduring constant discomfort.
Walking, swimming, or cycling contribute to cardiovascular health and endurance improvement without undue stress on the spine. Exercise can diminish inflammation, render ligaments and fascia more flexible, and reduce swelling, thereby lessening neurovascular compression.
While Lumbar Spinal Stenosis can be a disabling condition, multiple treatment options can significantly enhance a patient's quality of life. Patients might avoid surgical procedures and lessen their dependence on pharmaceutical interventions through appropriate exercise and manual therapy, leading to superior long-term results.
DR. BRIAN ABELSON, DC. - The Author

With over 30 years of clinical experience and a track record of treating more than 25,000 patients, Dr. Abelson developed the Motion Specific Release (MSR) Treatment Systems to provide powerful and effective solutions for musculoskeletal issues.
As an internationally best-selling author, he is passionate about sharing knowledge and techniques that can benefit the broader healthcare community. A perpetual student, Dr. Abelson continually integrates cutting-edge methods into the MSR programs, with a strong emphasis on multidisciplinary and patient-centered care.
Beyond his professional life, Dr. Abelson is a dedicated husband and father of two. He and his wife share a deep love for international travel, immersing themselves in different cultures, music, and the joy of connecting with people around the world. An Ironman triathlete and marathon runner for over 30 years, he is also a committed environmentalist with a passion for human rights. His practice, Kinetic Health, is based in Calgary, Alberta, Canada.
References:
Bussières, A., Cancelliere, C., & Ammendolia, C. (2021). Non-Surgical Interventions for Lumbar Spinal Stenosis Leading To Neurogenic Claudication: A Clinical Practice Guideline. J Pain, 22(9), 1015-1039. doi: 10.1016/j.jpain.2021.03.147.
Anderson, D.B., Luca, K., Jensen, R.K., et al. (2021). A critical appraisal of clinical practice guidelines for the treatment of lumbar spinal stenosis. Spine J, 21(3), 455-464. doi: 10.1016/j.spinee.2020.10.022.
Young, J.J., Hartvigsen, J., Roos, E.M., Ammendolia, C., Kongsted, A., Skou, S.T., Grønne, D.T., & Jensen, R.K. (2021). Symptoms of lumbar spinal stenosis in people with knee or hip osteoarthritis or low back pain: a cross-sectional study of 10,234 participants in primary care. Osteoarthritis Cartilage, 29(11), 1515-1520. doi: 10.1016/j.joca.2021.07.012.
Lurie, J., & Tomkins-Lane, C. (2016). Management of lumbar spinal stenosis. BMJ, 352, h6234. doi: 10.1136/bmj.h6234.
Deer, T.R., Grider, J.S., Pope, J.E., et al. (2019). The MIST Guidelines: The Lumbar Spinal Stenosis Consensus Group Guidelines for Minimally Invasive Spine Treatment. Pain Pract, 19(3), 250-274. doi: 10.1111/papr.12744.
Jensen, R.K., Harhangi, B.S., Huygen, F., Koes, B. (2021). Lumbar spinal stenosis. BMJ, 373, n1581. doi: 10.1136/bmj.n1581.
Rousing, R., Jensen, R.K., Fruensgaard, S., Strøm, J., et al. (2019). Danish national clinical guidelines for surgical and nonsurgical treatment of patients with lumbar spinal stenosis. Eur Spine J, 28(6), 1386-1396. doi: 10.1007/s00586-019-05987-2.
Schneider, M.J., Ammendolia, C., Murphy, D.R., et al. (2019). Comparative Clinical Effectiveness of Nonsurgical Treatment Methods in Patients With Lumbar Spinal Stenosis. JAMA Netw Open, 2(1), e186828.
Thistle, S. (2022). Older & Bolder: Chiropractic Care for Healthy Aging. Calgary.
Lundby, C., & Jacobs, R.A. (2016). Adaptations of Skeletal Muscle Mitochondria to Exercise Training. Experimental Physiology, 101 (1), 17-22.
Abelson, B.J., & Abelson, K.T. (2010). Exercises for the Jaw to Shoulder – Copyright Canada. Rowan Tree Books Ltd. ISBN (978-0-97338484-0).
Disclaimer:
The content on the MSR website, including articles and embedded videos, serves educational and informational purposes only. It is not a substitute for professional medical advice; only certified MSR practitioners should practice these techniques. By accessing this content, you assume full responsibility for your use of the information, acknowledging that the authors and contributors are not liable for any damages or claims that may arise.
This website does not establish a physician-patient relationship. If you have a medical concern, consult an appropriately licensed healthcare provider. Users under the age of 18 are not permitted to use the site. The MSR website may also feature links to third-party sites; however, we bear no responsibility for the content or practices of these external websites.
By using the MSR website, you agree to indemnify and hold the authors and contributors harmless from any claims, including legal fees, arising from your use of the site or violating these terms. This disclaimer constitutes part of the understanding between you and the website's authors regarding the use of the MSR website. For more information, read the full disclaimer and policies in this website.








Comments